Microplastics—tiny fragments of plastic less than 5 millimeters in length—have emerged as pervasive pollutants in aquatic and terrestrial environments. Recent research reveals a concerning link between these persistent particles and the acceleration of antibiotic resistance among bacterial communities. Antibiotic resistance poses one of the gravest threats to global public health, undermining decades of medical advances. When microplastics enter ecosystems, they not only act as physical contaminants but also serve as hotspots for bacterial colonization and genetic exchange. This article delves into the mechanisms by which microplastics promote antibiotic resistance, summarizes key study findings, explores the broader environmental and health implications, and outlines potential mitigation strategies.
What Are Microplastics?
Microplastics originate from two primary sources:
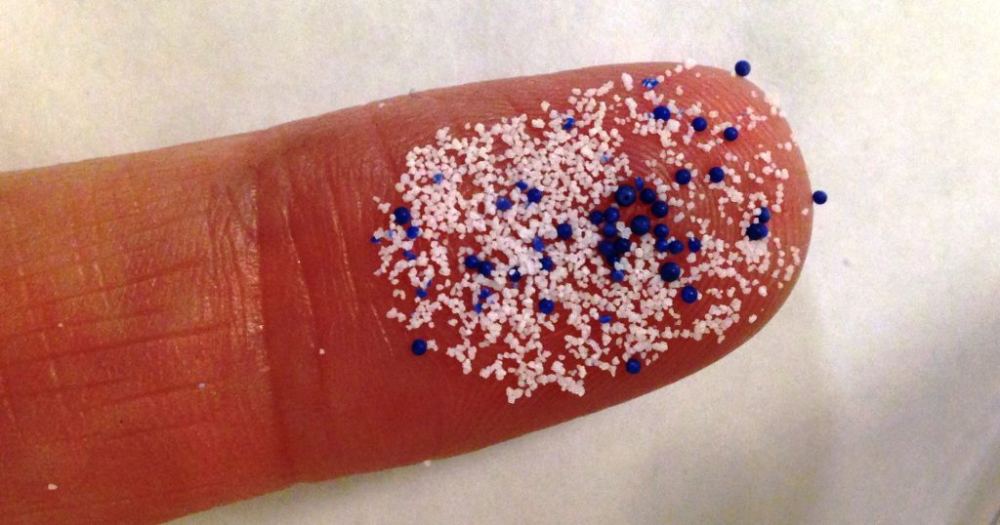
A. Primary Microplastics
-
Manufactured intentionally for use in products such as cosmetics, personal care items, and industrial abrasives.
-
Examples include microbeads in facial scrubs and pre-production plastic pellets (nurdles).
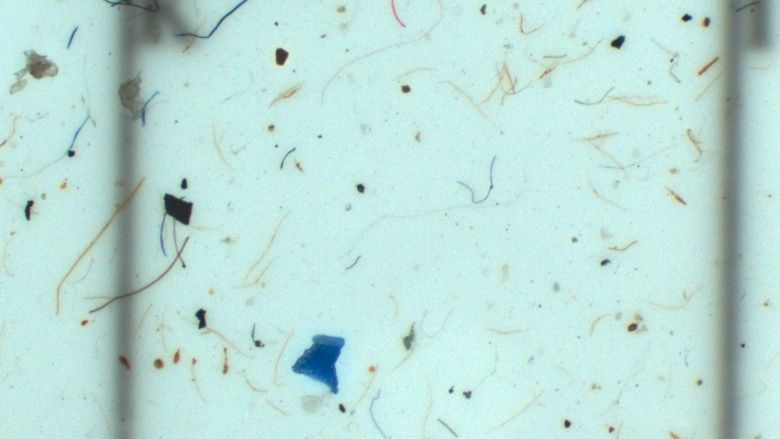
B. Secondary Microplastics
-
Result from the fragmentation of larger plastic debris due to photodegradation, mechanical abrasion, and chemical breakdown.
-
Common sources include degraded plastic bags, bottles, and fishing nets.
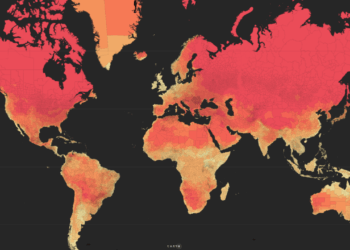
C. Environmental Ubiquity
-
Found in oceans, rivers, soils, and even the atmosphere.
-
Detected in tap water, bottled water, seafood, and agricultural soils.
Antibiotic Resistance: A Global Crisis
Antibiotic resistance arises when bacteria evolve mechanisms to survive exposure to antibiotics designed to kill or inhibit them. Key drivers include:
A. Overuse of Antibiotics
-
In human medicine through unnecessary prescriptions.
-
In agriculture for growth promotion and disease prevention in livestock.
B. Incomplete Treatment Courses
-
Patients failing to finish prescribed antibiotic regimens, allowing partially resistant strains to survive and proliferate.
C. Environmental Dissemination
-
Antibiotics and resistant bacteria enter water bodies through pharmaceutical manufacturing discharge, hospital effluent, and agricultural runoff.
Antibiotic-resistant infections claim hundreds of thousands of lives annually and threaten to reverse gains in treating previously curable diseases.
Linking Microplastics with Antibiotic Resistance
A groundbreaking study published in Environmental Science & Technology (2025) has shed light on how microplastics harbor and amplify antibiotic-resistant bacteria (ARB) and antibiotic-resistance genes (ARGs). Key findings include:
A. Biofilm Formation on Microplastics
-
Microplastics provide surfaces for bacterial biofilms—a complex aggregation of microorganisms embedded in an extracellular matrix.
-
Within biofilms, bacteria are more likely to exchange genetic material, including ARGs, via horizontal gene transfer (conjugation, transformation, transduction).
B. Concentration of Pollutants
-
Hydrophobic surfaces of microplastics adsorb antibiotics and other organic contaminants, creating localized hubs of selective pressure.
-
Sub-inhibitory concentrations of antibiotics on microplastic surfaces foster the development of resistant strains rather than killing susceptible ones outright.
C. Reservoirs for Pathogens
-
Studies demonstrate that microplastics can transport human and animal pathogens across vast distances, extending the geographic reach of ARB.
Mechanisms of Resistance Propagation
Bacteria on microplastics exploit several mechanisms to acquire and disseminate resistance genes:
-
Conjugation
-
Direct transfer of plasmids between bacterial cells within the biofilm.
-
-
Transformation
-
Uptake of free DNA fragments released by lysed cells, facilitated by the sticky biofilm matrix.
-
-
Transduction
-
Bacteriophages (viruses that infect bacteria) can transfer ARGs between bacteria in close proximity within biofilms.
-
Additionally, environmental stressors concentrated on microplastic surfaces—notably heavy metals and persistent organic pollutants—can co-select for antibiotic resistance through mechanisms of cross-resistance and co-resistance.
Environmental Impact
The intersection of microplastics and antibiotic resistance has cascading effects on ecosystem health:
A. Aquatic Ecosystems
-
Phytoplankton and zooplankton ingest microplastics, disrupting food webs and potentially transferring ARB to higher trophic levels.
B. Soil Microbiomes
-
Agricultural use of sludge and compost containing microplastics introduces ARGs into soil, impacting nutrient cycling and plant-associated microbial communities.
C. Wildlife Health
-
Ingestion of microplastics by fish, birds, and mammals can lead to gastrointestinal disturbances and act as vectors for ARB, posing risks to wildlife and human consumers.
Human Health Implications
Humans encounter microplastics and ARB through multiple pathways:
A. Drinking Water
-
Studies detect microplastic particles in both municipal tap water and bottled water, potentially carrying bacteria from source to tap.
B. Seafood Consumption
-
Filter-feeding organisms accumulate microplastics and associated bacteria, introducing ARB into human diets.
C. Airborne Inhalation
-
Atmospheric transport of microplastics containing ARB poses inhalation risks, though research is still emerging in this area.
Consequences of exposure to ARB include reduced efficacy of antibiotic treatments, prolonged hospital stays, and increased healthcare costs.
Mitigation Strategies
Addressing microplastics-fueled antibiotic resistance requires integrated measures:
A. Source Reduction
-
Ban or limit the use of primary microplastics in consumer products.
-
Improve waste management to minimize plastic litter and fragmentation.
B. Advanced Wastewater Treatment
-
Implement tertiary treatment technologies—such as membrane bioreactors and advanced oxidation processes—that remove microplastics and ARGs more effectively.
C. Green Infrastructure
-
Construct wetlands and biofiltration systems to intercept microplastics and contaminants before they enter natural water bodies.
D. Antibiotic Stewardship
-
Enforce strict guidelines for antibiotic prescription in healthcare and restrict non-therapeutic use in agriculture.
-
Educate stakeholders on complete treatment adherence and resistance risks.
E. Monitoring and Research
-
Develop standardized methods for detecting microplastics and ARGs in environmental samples.
-
Fund longitudinal studies to assess the long-term impacts of microplastics on microbial ecology and resistance patterns.
Policy and Governance
Strong policy frameworks can drive change:
A. International Agreements
-
Expand global treaties—such as the Basel Convention—to include microplastics and their role in spreading ARB.
-
Harmonize regulations on plastic production, disposal, and antibiotic usage.
B. National Legislation
-
Enact bans on microbeads and set limits on microplastic discharge from industrial sources.
-
Fund research grants focused on pollution microbiology and resistance mitigation.
C. Public-Private Partnerships
-
Encourage collaboration between governments, NGOs, and industry to innovate biodegradable alternatives and sustainable packaging.
Conclusion
The convergence of microplastic pollution and antibiotic resistance represents a multifaceted threat to environmental integrity and human health. Microplastics act as mobile platforms that concentrate pollutants and foster genetic exchanges among bacteria, accelerating the rise of antibiotic-resistant strains. Combating this challenge demands a holistic approach—encompassing source reduction, technological upgrades in wastewater treatment, antibiotic stewardship, robust monitoring, and cohesive policy measures. By acknowledging and addressing the role of microplastics in antibiotic resistance, stakeholders can safeguard the efficacy of life-saving drugs and protect ecosystems for future generations.