In recent years, microplastics have emerged as a pervasive environmental pollutant with far-reaching impacts. A groundbreaking study now reveals that these tiny particles may play a crucial role in accelerating antibiotic resistance among bacterial populations. This article delves into the mechanisms behind this phenomenon, explores the latest research findings, and discusses potential strategies to mitigate the risks. Whether you are an environmental enthusiast, public health advocate, or policy maker, understanding the link between microplastics and antibiotic resistance is essential in tackling one of today’s most pressing challenges.
Section 1: What Are Microplastics? Microplastics are plastic fragments measuring less than 5 millimeters in diameter. They originate from two primary sources:
A. Primary Microplastics: Manufactured intentionally for products such as microbeads in personal care items.
B. Secondary Microplastics: Resulting from the breakdown of larger plastic debris under environmental stressors like UV radiation and mechanical abrasion.
These particles are ubiquitous in oceans, rivers, soils, and even the atmosphere. Their small size enables them to travel long distances, infiltrate food chains, and persist in ecosystems for decades. Due to their pervasiveness, humans are now inadvertently consuming microplastics through food, water, and air, raising further concerns about their health implications.
In marine environments, microplastics often aggregate with organic matter and serve as vectors for various chemical contaminants. They are ingested by plankton, fish, and marine mammals, gradually making their way up the food chain. This bioaccumulation has profound ecological consequences, as it alters feeding behaviors, reproductive functions, and survival rates among aquatic species.
Section 2: Antibiotic Resistance – A Growing Threat Antibiotic resistance occurs when bacterial strains evolve to survive exposure to antibiotics that would normally inhibit their growth or kill them.
This resistance is facilitated by genetic mutations and horizontal gene transfer (HGT) mechanisms such as transformation, transduction, and conjugation. Key drivers include:
A. Overuse of antibiotics in medicine and agriculture.
B. Improper disposal of pharmaceutical waste into waterways.
C. Lack of new antibiotic development due to economic and regulatory challenges.
D. Inadequate infection prevention and control in healthcare settings.
According to the World Health Organization, antibiotic resistance represents one of the top ten global public health threats. It is estimated that by 2050, antibiotic-resistant infections could result in 10 million deaths annually and cost the global economy over $100 trillion. Common illnesses such as urinary tract infections, pneumonia, and bloodstream infections are increasingly becoming harder to treat due to rising resistance.
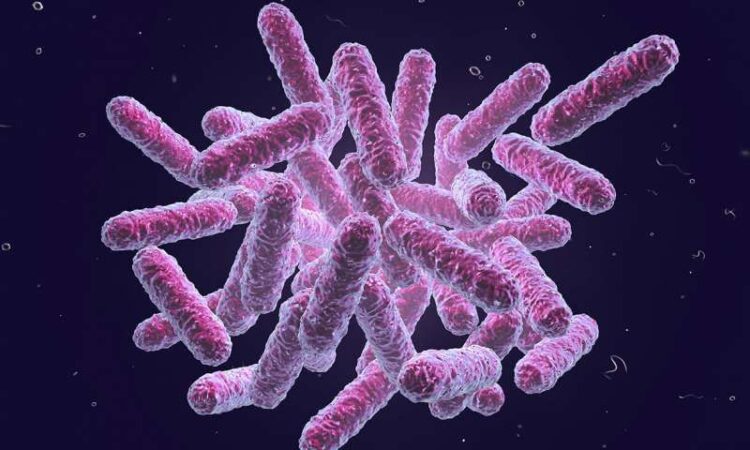
Section 3: How Microplastics Promote Antibiotic Resistance Recent research has illuminated several pathways through which microplastics exacerbate antibiotic resistance:
A. Surface for Biofilm Formation: Microplastics provide a scaffold for bacterial colonization. Biofilms are dense microbial communities embedded in a self-produced matrix. These biofilms enable close bacterial proximity, facilitating horizontal gene transfer of resistance genes, particularly through conjugation.
B. Pollutant Adsorption: Chemical residues, including antibiotics, heavy metals, and persistent organic pollutants (POPs), adhere to microplastic surfaces. These adsorbed pollutants create micro-environments with elevated selective pressure, encouraging the proliferation of resistant bacteria.
C. Vector for Pathogens: Transported over long distances by wind and water currents, microplastics can carry resistant bacteria across geographical boundaries. This increases the likelihood of resistant genes spreading between ecosystems and populations.
D. Induction of Stress Responses: Exposure to microplastics induces oxidative stress in bacteria, which in turn may trigger mechanisms that enhance mutagenesis and gene exchange.
Section 4: Key Study Insights A landmark study published in Environmental Science & Technology examined coastal waters and found:
A. Higher concentrations of antibiotic-resistant bacteria on microplastic surfaces compared to surrounding water.
B. Elevated levels of resistance genes such as bla_TEM_ and tet_M_ in biofilm communities.
C. Correlation between microplastic density and resistance gene abundance.
Researchers collected samples from five coastal sites over six months, employing metagenomic sequencing to analyze microbial communities. The findings underscore the role of microplastics as reservoirs and vectors for resistance. The study also revealed that microplastics facilitate the coexistence of multiple resistant strains, fostering the development of multi-drug-resistant bacteria.
Further, microplastics collected from urban areas showed significantly higher loads of resistant genes compared to those from remote regions. This suggests that anthropogenic activities, such as wastewater discharge and industrial pollution, exacerbate the issue.
Section 5: Environmental and Health Implications The fusion of microplastic pollution and antibiotic resistance poses multifaceted risks:
A. Ecosystem Disruption: Altered microbial community dynamics may affect nutrient cycling, biogeochemical processes, and food web stability. The decline in beneficial microbes and the rise in pathogenic strains could have cascading effects on biodiversity.
B. Human Exposure: Microplastics and associated resistant bacteria have been detected in drinking water, seafood, table salt, and even airborne dust. Ingested microplastics can accumulate in the gastrointestinal tract and potentially disrupt gut microbiota.
C. Public Health Crisis: Increased incidence of hard-to-treat infections could overwhelm healthcare systems, especially in low-resource settings. The spread of resistance genes through environmental vectors may undermine current infection control strategies.
D. Economic Burden: Treating resistant infections is costlier and requires prolonged hospital stays, expensive drugs, and intensive care, placing significant financial strain on individuals and health systems.
Section 6: Mitigation Strategies Combating this dual threat requires coordinated actions across multiple sectors: A. Source Reduction:
- Phase out microbeads in personal care products through legislative bans.
- Promote the reduction, reuse, and recycling of plastic materials.
- Encourage industries to adopt eco-friendly packaging solutions. B. Regulatory Measures:
- Enforce stricter limits on antibiotic discharge from pharmaceutical and agricultural facilities.
- Implement guidelines for prudent antibiotic use in livestock and aquaculture.
- Monitor and regulate microplastic emissions from urban runoff and wastewater. C. Technological Innovations:
- Develop biodegradable alternatives to conventional plastics using materials such as polylactic acid (PLA), polyhydroxyalkanoates (PHA), and starch-based polymers.
- Utilize advanced filtration systems, including membrane bioreactors and nanotechnology, to remove microplastics and pathogens from wastewater.
- Invest in real-time monitoring technologies for detecting resistance genes in environmental samples. D. Public Awareness and Education:
- Conduct public campaigns to raise awareness about the impacts of plastic pollution and antibiotic misuse.
- Educate healthcare professionals, veterinarians, and farmers on antimicrobial stewardship principles.
- Integrate environmental health topics into school curricula to cultivate responsible behaviors from an early age.
Section 7: Case Studies and Policy Examples Several countries have taken proactive steps:
- The European Union has banned microbeads and is working on comprehensive plastic legislation.
- Sweden and Norway have stringent regulations on pharmaceutical waste disposal.
- China is investing in bioplastics research and has implemented strict controls on antibiotic use in farming.
Collaborative international efforts such as the United Nations Environment Programme (UNEP) and the Global Action Plan on Antimicrobial Resistance are essential in driving global change.
Section 8: Future Research Directions Scientists recommend further investigations into: A. Long-term monitoring of microplastic-associated resistance in diverse environments, including terrestrial and atmospheric systems. B. Interaction effects between microplastics, emerging pollutants, and microbial communities. C. Efficacy of novel remediation technologies in real-world settings. D. Development of biodegradable plastics that do not foster biofilm formation or gene exchange. E. Quantitative risk assessments to evaluate human exposure pathways and health outcomes.
Interdisciplinary research combining microbiology, environmental science, chemistry, and public health is vital to deepen our understanding and inform evidence-based interventions.
Conclusion
The intersection of microplastic pollution and antibiotic resistance represents a critical environmental and public health challenge. The latest study underscores the urgent need for holistic strategies that address both plastic contamination and antibiotic misuse. As the world grapples with escalating antibiotic resistance and plastic waste, coordinated global action is imperative. By combining policy reforms, technological advances, and community engagement, we can work towards safeguarding ecosystems and human health.
Through continuous research, responsible consumption, and regulatory vigilance, it is possible to curb the rise of resistant pathogens and reduce the ecological footprint of plastic pollution. The time to act is now, before the synergistic threats of microplastics and antibiotic resistance spiral beyond control.