Air pollution remains one of the most pressing environmental health challenges worldwide. While its links to respiratory and cardiovascular diseases are well documented, growing evidence points to a troubling connection between polluted air and male reproductive health. This article examines how airborne contaminants contribute to declining sperm quality, increased infertility rates, and broader implications for public health and policy.
1. Understanding Air Pollution: Sources and Composition
A. Primary Pollutants: Emitted directly from sources like vehicle exhaust, industrial chimneys, and construction sites. Common examples include particulate matter (PM), nitrogen oxides (NOx), sulfur dioxide (SO₂), and volatile organic compounds (VOCs).
B. Secondary Pollutants: Formed in the atmosphere through chemical reactions. Ground-level ozone (O₃), for instance, results from NOx and VOCs interacting under sunlight.
C. Particulate Matter Categories:
- PM₁₀: Particles with diameters of 10 micrometers or less, capable of entering respiratory passages.
- PM₂.₅: Even finer particles (≤2.5 μm) that penetrate deep into lung tissue and enter the bloodstream.
2. Mechanisms of Reproductive Toxicity
A. Oxidative Stress
- Pollutants generate reactive oxygen species (ROS) that damage sperm DNA, proteins, and lipids.
- ROS overproduction overwhelms antioxidant defenses, leading to cell dysfunction and death.
B. Endocrine Disruption
- Certain contaminants mimic or block hormones, altering testosterone production and signaling.
- Phthalates and polycyclic aromatic hydrocarbons (PAHs) are among the chemicals implicated in hormone imbalance.
C. Inflammatory Pathways
- Inhaled toxins provoke systemic inflammation, raising cytokine levels that can impair testicular function.
- Chronic inflammation disrupts the blood-testis barrier, compromising sperm development.

3. Epidemiological Evidence of Impact on Male Fertility
A. Decline in Semen Quality Over Time
- Multiple studies report a downward trend in sperm concentration and motility over the past decades in urban populations.
- Example: Researchers in metropolitan areas documented a 30% reduction in average sperm count between 1990 and 2020.
B. Associations with Specific Pollutants
- Elevated PM₂.₅ exposure correlates with lower sperm motility and abnormal morphology.
- Increased traffic-related NO₂ levels link to decreased sperm concentration in several cohort studies.
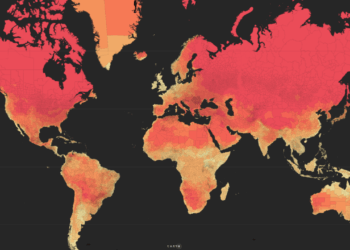
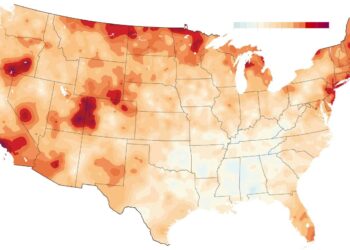
C. Geographical Variations
- Fertility parameters tend to be poorer in regions with persistent smog and heavy industrial activity compared to rural zones.
- Seasonal fluctuations: Semen quality often falls during high-pollution months.
4. Laboratory and Animal Model Findings
A. In Vitro Experiments
- Human sperm samples exposed to common urban air mixtures show dose-dependent decreases in viability.
- Antioxidant supplementation in vitro can partially rescue pollutant-induced damage.
B. Rodent Studies
- Male rats subjected to concentrated ambient particles exhibit reduced sperm count and testicular weight.
- Markers of oxidative stress and apoptosis are elevated in testicular tissue of exposed animals.
C. Transgenerational Effects
- Evidence suggests that paternal exposure to pollutants may affect offspring fertility via epigenetic changes.
- Altered DNA methylation patterns observed in sperm of exposed rodents.
5. Broader Health and Societal Implications
A. Public Health Burden
- Infertility affects approximately 15% of couples globally; male factors contribute to nearly half of these cases.
- Air pollution may account for a significant, yet underrecognized, fraction of male infertility.
B. Economic Costs
- Reduced workforce fertility leads to demographic shifts, increased healthcare spending on assisted reproductive technologies, and lost productivity.
C. Environmental Justice Considerations
- Disadvantaged communities often face higher pollution levels and have limited access to fertility care.
- Policy interventions must address these inequities to ensure reproductive health for all populations.

6. Mitigation Strategies and Recommendations
A. Individual-Level Actions
- Avoid outdoor exercise during peak pollution hours.
- Use indoor air purifiers with HEPA filters.
- Maintain a diet rich in antioxidants (e.g., vitamins C and E).
B. Community and Policy Initiatives
- Strengthen air quality regulations targeting vehicle emissions and industrial discharges.
- Expand urban green spaces to capture particulate matter and improve local air quality.
- Encourage use of public transit, cycling, and electric vehicles.
C. Research and Surveillance
- Implement longitudinal fertility registries linked to environmental exposure data.
- Fund studies on pollutant mixtures and mixtures’ reproductive effects.
Conclusion
The evidence linking air pollution to male infertility is mounting and multifaceted. From oxidative damage and hormonal disruption to systemic inflammation, airborne toxins compromise sperm health and reproductive outcomes. Addressing this silent threat requires coordinated efforts at individual, community, and policy levels. By reducing emissions, improving air quality, and supporting further research, we can safeguard male fertility and promote healthier future generations.